Urine Problem
Permanent Curable By Ayurvdic Medicine
( आयुर्वेदिक दवाओं द्वारा स्थाई इलाज संभव )
If you’re like many men, you have experienced some changes in your urination—or even had problems urinating—as you’ve gotten older. And, like your peers, you may not have given these issues much thought, instead chalking them up to general signs of aging like a few grey hairs and a tougher time keeping your 8-minute-mile running record.
A weak urine stream may not be at the top of your list of things to attend to (or discuss), but your doctor can help you get the right treatment, if any is needed, to improve your symptoms. (Yes, you may finally be able to make it through the night without six trips to the bathroom.)
Listen to the messages your body is sending you. If you notice symptoms such as excessive thirst, pain during urination, fever, abdominal or back pain, insomnia, daytime fatigue, memory loss or depression, don’t wait to seek medical advice. These, paired with urination issues, could be a sign of something more serious, such as bladder stones or prostate cancer.
Below are a few common concerns, possible causes and recommended solutions.
Your Stream is Weak or You Can’t Go When You Try
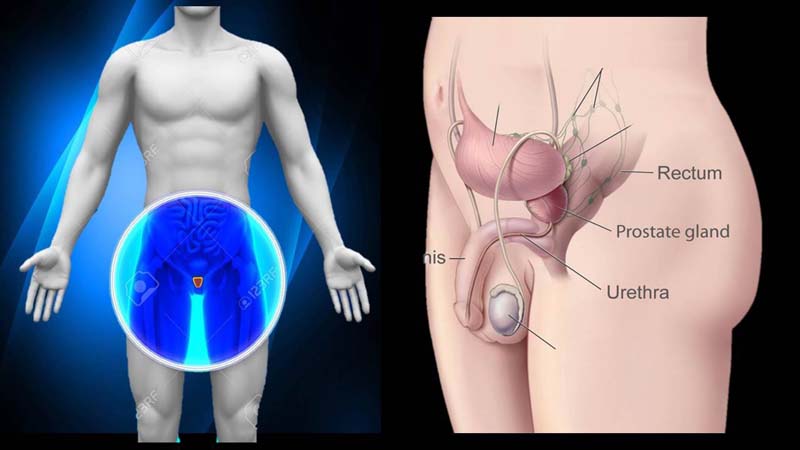
This problem is often due to an increase in prostate gland cells—called enlarged prostate, or benign prostatic hyperplasia (BPH)—which tends to affect men beginning at around age 40. It becomes even more common as men age, affecting 90 percent of men age 80 and older.
The increase in the gland’s size, normally comparable to a walnut, may cause it to push on and narrow the nearby urethra—a thin tube that urine passes through on its way from the bladder to the tip of the penis. This can slow down how quickly urine passes, contributing to urination hesitancy—a weak stream, dribbling or straining to go, even though you feel the urge.
The prostate itself, which is made up of smooth muscles, can contract involuntarily and compress the urethra in a similar way. Constipation may also be a culprit, since hard stool can cause the rectum to push against the bladder and urethra, causing or aggravating BPH.
It’s worth seeing your doctor if you have these symptoms, because a prescription or some simple lifestyle changes may be all that’s needed to improve them. Tell your doctor about all medications you are taking, as they could be affecting your urination as well. (Antihistamines, decongestants and antidepressants are common culprits.) An alternative medication may help.
When BPH and medication aren’t to blame, an underlying health issue such as a prostatic infection or a urethral infection (often from a sexually transmitted disease), bladder stones or even prostate or bladder cancer could be. Your doctor may recommend blood and urine samples, or an X-ray, ultrasound, digital rectal exam or colonoscopy to investigate further.
You Have to Go… Even Though You Just Went
The urge to use the bathroom frequently—and suddenly—throughout the day can be a sign of an overactive bladder, or involuntary bladder contractions. This leads to unintentional urine leakage and the need to urinate more than eight times in 24 hours.
An overactive bladder may be related to advanced age, BPH, prostate surgery or a medication that you are taking, such as a diuretic or lithium. In these cases, your physician may stop or change your medication or prescribe one that can help relax the bladder or reduce urine production, and recommend alternatives to your meds (if applicable and possible).
You can take some steps on your own to help, too:- Spread fluid consumption throughout your day to prevent your bladder from becoming overloaded (which may help you make it through your next movie with a few less trips to the restroom).
- To regulate the urination process, try exercising your pubococcygeal muscles, which support the pelvic floor and surround the penis. Regularly contracting them (which can be done anywhere, anytime) helps build their strength, minimizing leakage and improving urine control. Begin with 10 to 20 “flexes” (called Kegels) a day and work up to 100. You will know that you’re working the right muscles when it feels just like it does when you’re trying to stop peeing.
These treatments are typically sufficient for most people, but if they aren’t effective, your doctor may suggest more aggressive solutions, such as stimulation of the sacral nerves (those that carry signals between your spinal cord and your bladder’s tissue) or surgery.
Other possible causes of a frequent need to urinate can include diabetes, bladder cancer, stroke and other neurological conditions, so your doctor may recommend additional testing if overactive bladder has been ruled out.
You Get Up to Urinate at Least a Few Times Each Night
Getting up to urinate at least twice during the night, an increased quantity of urine every time you go or a combination of these issues may mean that you are experiencing nocturia, or chronic nighttime urination. Though more common in people with diabetes, or heart or liver failure, anyone can develop it. Some people may simply produce more urine while they sleep or experience a diminished capacity to hold urine in their bladder for long stretches.
If you suspect that a medication is causing nocturia, speak with your doctor about changing your dosage or trying an alternate prescription. Your doctor may prescribe medicine that relaxes the bladder, which can help minimize the number of trips you take to the bathroom at night.
In addition, these lifestyle strategies may improve your nighttime bladder control symptoms:
- Try to avoid drinking fluids two hours before bedtime to curb common nighttime issues like bed-wetting.
- Eliminate or reduce your consumption of caffeine and alcohol—especially after 7pm. Both are diuretics, which means they make you have to go more frequently.
Nocturia can also be the result of a bladder infection or inflammation, which can be quickly identified and treated by your doctor. Other times, it may be a symptom of other health issues including sleep apnea or bladder and prostate cancers. Urine analysis, ultrasound or sleep studies, among other tests, may be required to learn more.